Purposes of Diagnosis
1. Confirm the etiology of disease in cats with clinical signs and/or clinicopathological abnormalities compatible with FeL (Figure 15)
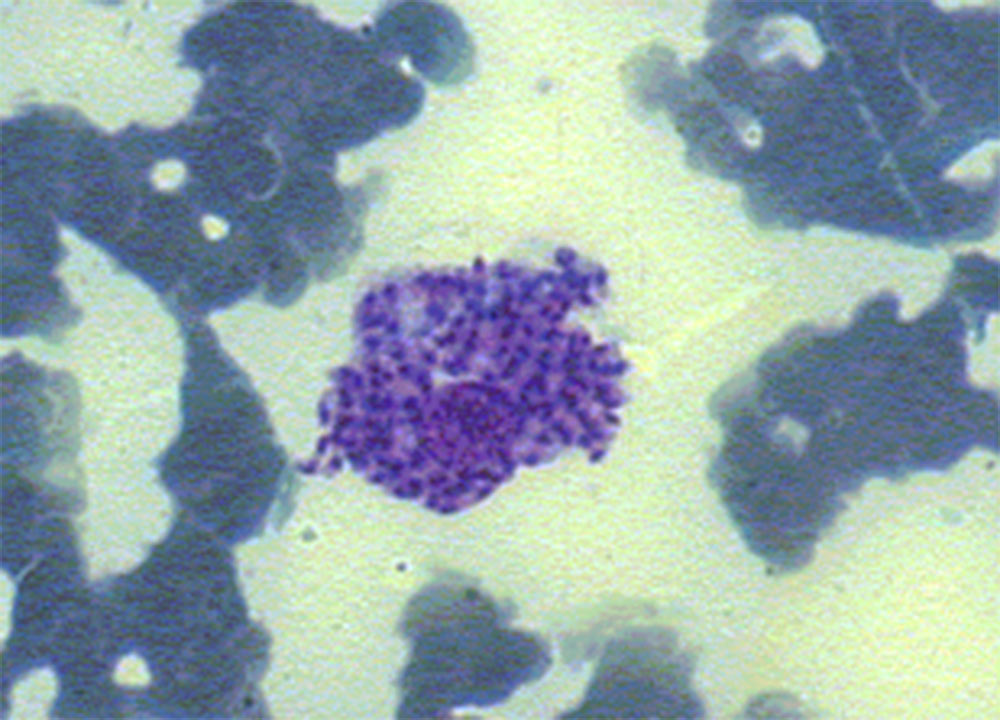
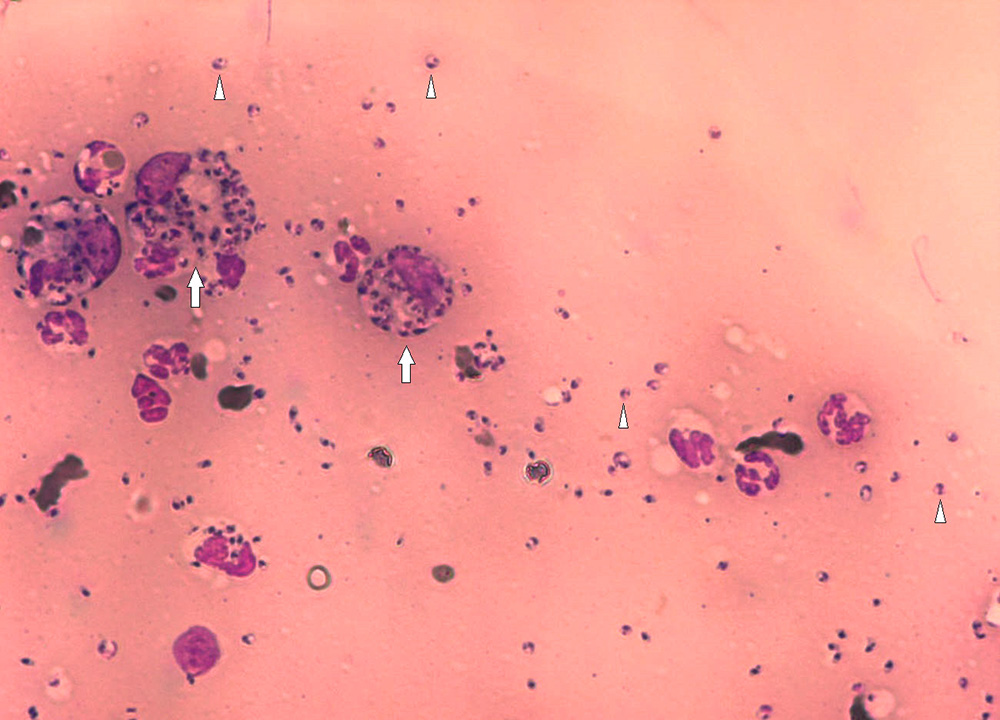
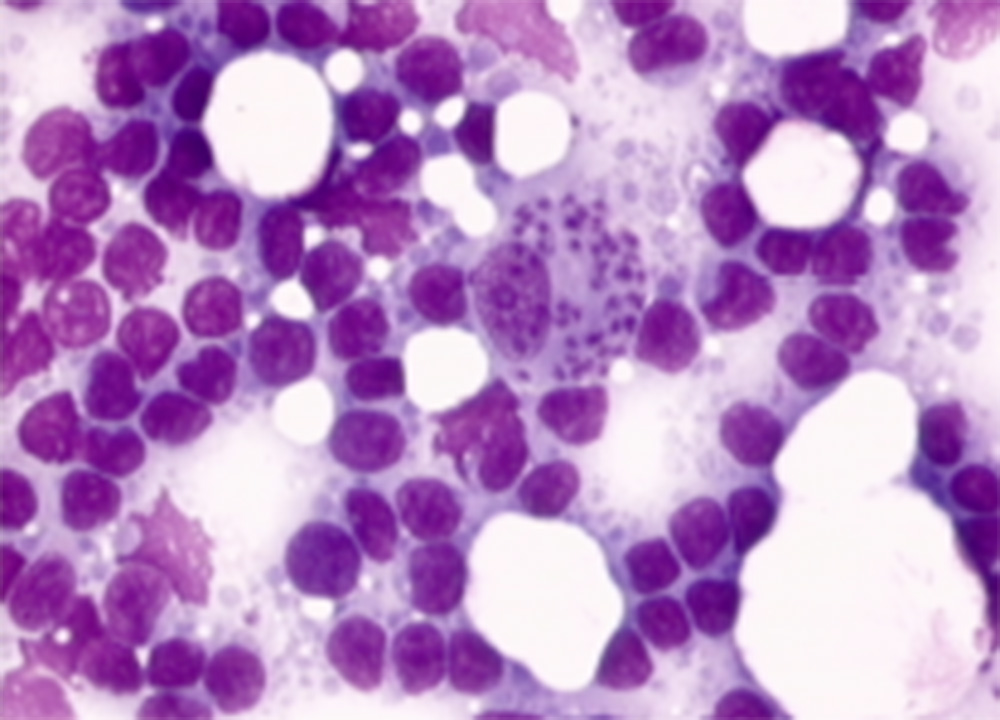
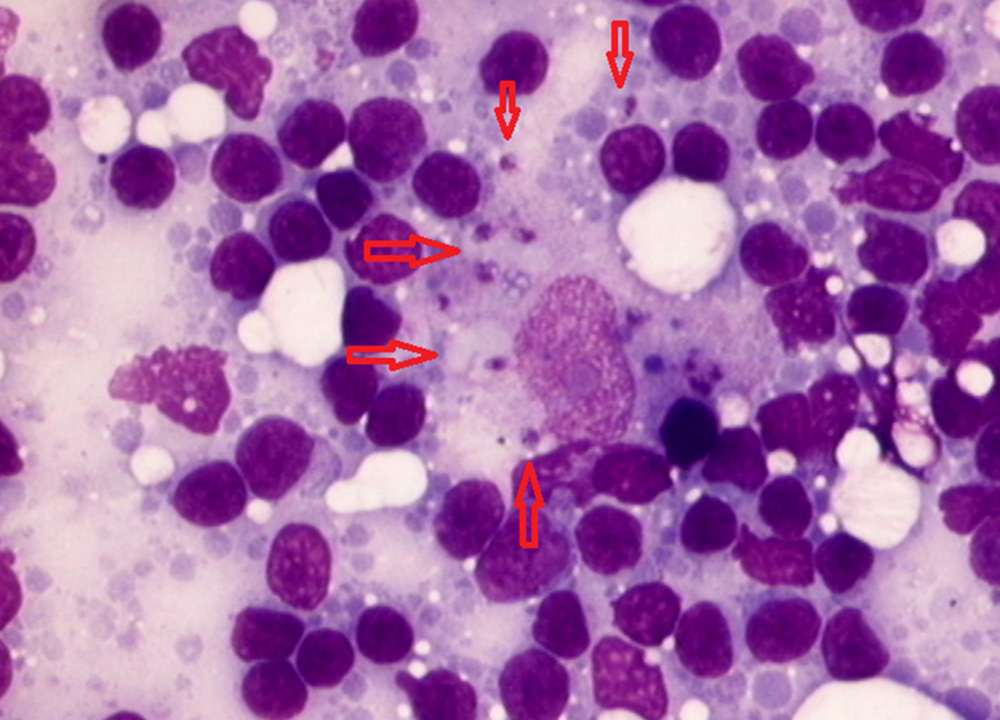
High levels of antibody positivity (i.e. in case of IFAT > 3 dilutions over the validated cut-off value) detected by quantitative serology (IFAT, ELISA or DAT) confirm diagnosis in cats with a risk of exposure to L. infantum infection and suggestive clinical signs and/or clinicopathological abnormalities (Table 1). However, cytological evaluation of any skin, mucosal, or mucocutaneous lesions, enlarged lymph nodes or spleen, or any other lesion evidenced by imaging and endoscopy should be performed. Compatible cytological findings (such as lymphoid hyperplasia in lymphoid organs; and neutrophilic and/or macrophagic as well as lymphoplasmocellular inflammation) and/or visualization of amastigotes is suggestive or confirmatory of L. infantum infection, respectively (Figures 11-14). Cytology also permits to detect comorbidities. Histopathological evaluation and/or Leishmania immunohistochemistry may be required based on each patient’s list of problems.
In antibody-negative or low-positive cats with no evidenced tissue lesions, Leishmania amastigotes (cytology evaluation) or parasite DNA (PCR) can be detected in bone marrow, lymph nodes or spleen. However, as comorbidities are possible, they also must be investigated based on the individual list of problems, to confirm a causative role of L. infantum infection in the clinical presentation (i.e. differentiation of infection from disease).
Point-of-care tests validated to detect anti-L. infantum antibodies in cats are currently not available.
2. Screening of apparently healthy cats living or travelling to or from endemic areas
The screening of clinically healthy cats by means of quantitative serology and PCR techniques is recommended in endemic areas in case of the following conditions: blood donors, cats requiring chronic immunosuppressive therapies, and before relocating cats to non-endemic areas. Imported/relocated cats must be tested at arrival, but seroconversion can take months and retesting should be considered six months later, in case of presenting compatible clinical signs, before any immunosuppressive therapy or becoming a blood donor. In case of healthy individuals, generally minimally invasive tissue sampling is preferred (blood, lymph nodes and conjunctival swabs) for PCR, however their sensitivity is low and it should be increased by performing multiple tissue PCR testing.
Figure 15. Flow chart for the diagnostic approach to cats with clinical signs compatible with FeL
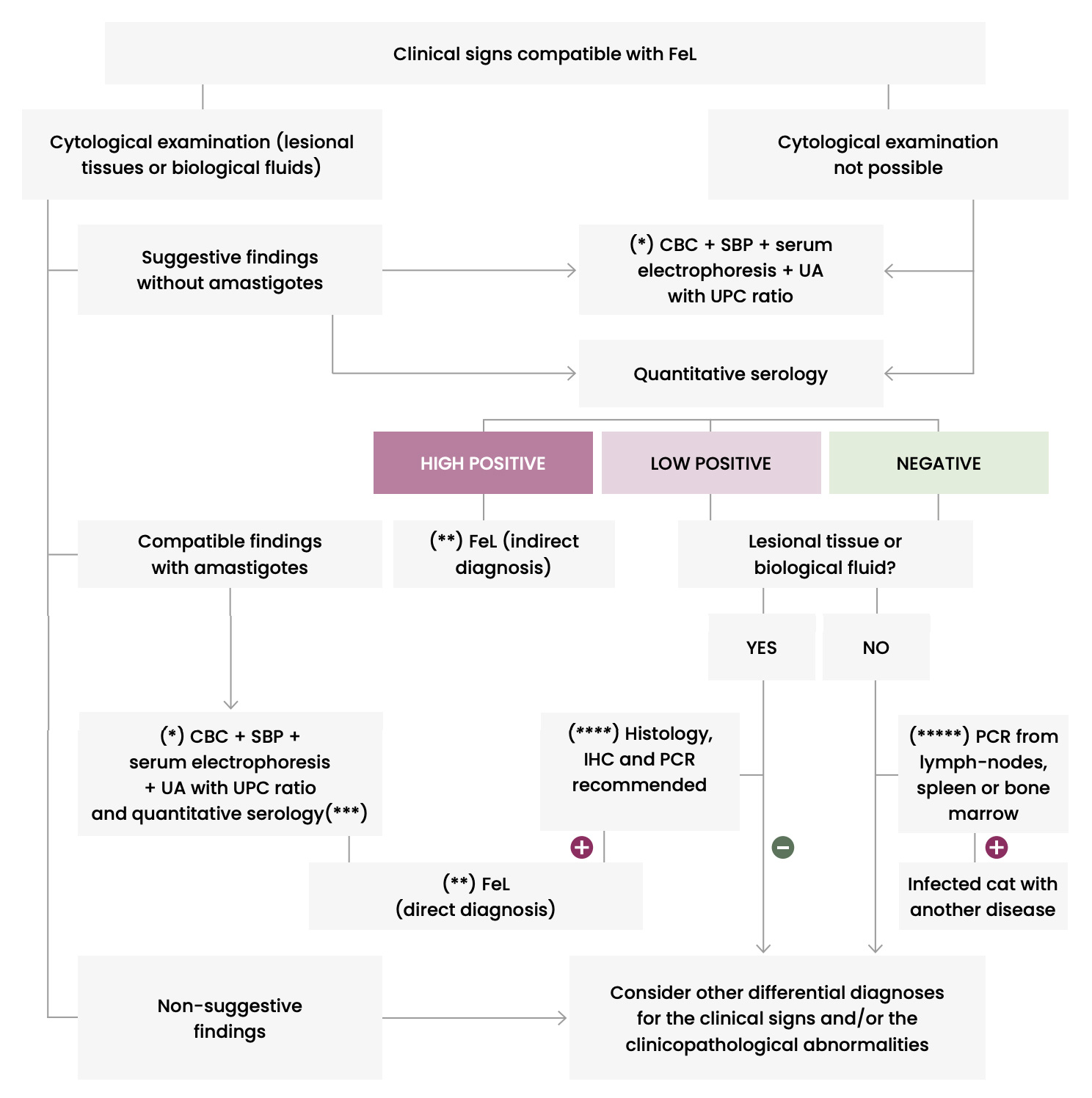
CBC: Complete blood count – IHC: Immunohistochemistry – PCR: Polymerase chain reaction – SBP: Serum biochemical profile – UA: Urinalysis – UPC: Urinary protein:creatinine ratio
(*) To better check health status and evaluate clinicopathological abnormalities suggestive of FeL.
(**) Conventional anti-Leishmania treatment and monitoring for resolution of clinical signs and clinicopathological abnormalities.
(***) Quantitative serology is recommended for the post-treatment follow-up.
(****) A cat will be considered with leishmaniosis if histopathological findings are compatible with leishmaniosis and IHC or PCR are positive. It is not common to visualize amastigotes in histology and therefore, IHC is always recommended. If IHC is negative, PCR is performed to confirm or rule out infection.
(*****) Detection of infection based on clinical suspicion.